1. What is Root Canal Treatment?
1.1 Definition and Purpose
Root canal treatment (RCT) is a dental procedure used to repair and save a tooth that is severely decayed or infected, often due to deep cavities or trauma. The procedure involves the removal of the infected or damaged pulp (the tissue inside the tooth), cleaning and disinfecting the pulp chamber and root canals, and then filling and sealing the empty space.
The primary goals of RCT are:
- To eliminate infection
- To relieve pain
- To restore the function of the tooth
- To prevent further infection or reinfection
1.2 The Anatomy of a Tooth
Understanding the anatomy of the tooth is essential to appreciating the importance of root canal treatment. A tooth consists of several layers:
- Enamel: The outer hard layer that protects the tooth.
- Dentin: The layer beneath the enamel that makes up the majority of the tooth’s structure.
- Pulp: The innermost part of the tooth, composed of nerves, blood vessels, and connective tissue.
- Root Canal: A system of narrow channels running through the root of the tooth that contains the pulp.
In RCT, the pulp and any infected tissue inside the root canal are removed, and the canals are cleaned and sealed to prevent further infection.
2. Indications for Root Canal Treatment
2.1 Primary Indications
Root canal therapy is recommended when the pulp of the tooth becomes infected or severely damaged. Common indications include:
- Severe Tooth Decay: When a cavity is too deep and extends into the pulp, causing infection or inflammation.
- Trauma: A cracked or fractured tooth can expose the pulp to bacteria, resulting in an infection.
- Persistent Tooth Pain: Unexplained or severe tooth pain, especially when biting or chewing, often indicates infection in the pulp.
- Abscess: The formation of an abscess or pus-filled pocket around the root, often caused by untreated infections, is a clear sign that root canal therapy is needed.
- Discoloration: A darkened or discolored tooth may be a sign of pulp necrosis (death of the pulp tissue).
2.2 Contraindications for Root Canal Treatment
While root canal therapy is highly effective, there are some situations where it may not be the ideal solution:
- Severe Tooth Damage: If the tooth is too damaged to support a crown or restoration, extraction may be a better option.
- Non-Viable Tooth: If the tooth’s roots are severely fractured, or if the tooth has been subjected to significant trauma beyond repair, RCT may not be feasible.
- Inadequate Bone Support: If the surrounding bone is significantly resorbed or damaged, the prognosis for a successful root canal may be poor.
- Systemic Health Issues: In some cases, if a patient has certain systemic health conditions that affect healing or increase infection risk, root canal therapy may need to be postponed or avoided.
3. The Root Canal Treatment Procedure
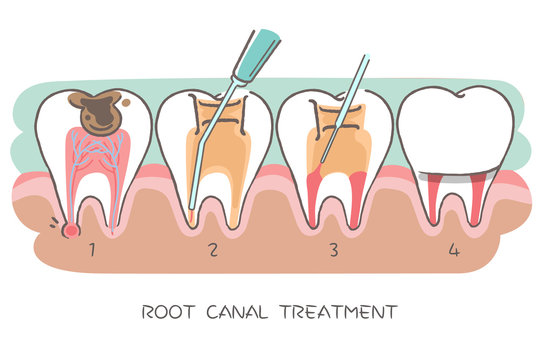
Root canal treatment involves several steps to clean and seal the infected tooth. Below are the key stages of the procedure:
3.1 Initial Consultation and Diagnosis
The process begins with a thorough clinical examination. The dentist or endodontist will assess the extent of the infection, check for visible signs of abscesses, and take X-rays to visualize the tooth’s root canals and surrounding bone structure. This information helps in formulating an appropriate treatment plan.
3.2 Local Anesthesia
Root canal treatment is typically performed under local anesthesia to ensure that the procedure is painless. The anesthetic is injected near the tooth being treated, numbing the area completely.
3.3 Access Opening
Once the anesthesia has taken effect, the dentist will create a small opening in the crown (top surface) of the tooth to access the pulp chamber and root canals. This is usually done using specialized dental tools, ensuring minimal damage to the surrounding tooth structure.
3.4 Cleaning and Shaping the Canals
Using small, flexible files, the dentist or endodontist will carefully remove the infected or damaged pulp tissue from the root canals. The canals are then cleaned and shaped to ensure they are free of bacteria and debris. This process may involve the use of irrigants, such as sodium hypochlorite, to disinfect the canals.
3.5 Filling the Canals
After cleaning, the root canals are dried and filled with a biocompatible material, such as gutta-percha, to seal the canals and prevent future infection. The tooth is then sealed with a temporary or permanent filling to protect it from contamination.
3.6 Final Restoration
In most cases, a tooth that has undergone root canal therapy requires a permanent restoration, such as a crown, to protect it from further damage and restore its function. The dentist will take impressions of the tooth to create the crown, which will be placed after the root canal procedure is complete.

4. Post-Treatment Care and Follow-up
4.1 Immediate Aftercare
After root canal therapy, patients may experience mild discomfort or sensitivity, which typically subsides within a few days. Over-the-counter pain relievers like ibuprofen or acetaminophen can help manage any post-treatment discomfort.
4.2 Follow-Up Appointments
A follow-up appointment is often scheduled to check the healing progress and ensure there are no signs of infection or complications. The dentist may take new X-rays to confirm that the root canal has been sealed properly.
5. Complications and Risks
While root canal therapy is highly effective, complications can arise in some cases. Some potential issues include:
- Reinfection: If the root canal was not properly sealed or if bacteria were not fully removed, reinfection can occur.
- Incomplete Treatment: Sometimes, due to complex canal anatomy or other factors, the root canals may not be completely cleaned or filled, leading to incomplete treatment.
- Tooth Fracture: Root canal therapy weakens the tooth structure, making it more prone to fractures, especially if a crown is not placed afterward.
- Anatomical Challenges: Some teeth have complex or curved root canal systems that are difficult to treat effectively, increasing the risk of complications.
6. Advancements in Root Canal Treatment
6.1 Technology in Root Canal Therapy
Modern root canal therapy has evolved with the introduction of several technologies aimed at improving treatment outcomes and patient comfort. Some of these advancements include:
- Microscopes: Dental microscopes allow endodontists to see the root canal system in greater detail, enhancing precision during the procedure.
- Digital X-rays: Digital imaging provides clearer, more accurate images, reducing radiation exposure and improving diagnostic capabilities.
- Rotary Endodontics: This technology uses motorized tools to clean and shape the root canals more efficiently than traditional manual methods.
- Laser Therapy: Lasers are sometimes used to disinfect the canals, providing enhanced bacteria removal and faster healing times.
6.2 Regenerative Endodontics
Regenerative endodontics is an emerging field that aims to regenerate damaged or infected pulp tissue using stem cells, growth factors, and scaffolds. While still in experimental stages, this technique holds promise for tooth revascularization and regeneration, particularly in younger patients with incomplete root development.
6.3 Bioceramic Materials
Bioceramic materials have been developed for root canal filling, offering better sealing properties and improved biocompatibility compared to traditional materials like gutta-percha. These materials are more resistant to bacterial leakage and provide a more favorable environment for healing.
7. Root Canal Treatment and the Role of the Dentist
Root canal therapy is a specialized procedure that often requires the expertise of an endodontist— a dentist who specializes in the diagnosis and treatment of dental pulp diseases. However, general dentists are also trained to perform routine root canal procedures on simple cases.
It is important for patients to select a skilled and experienced dentist or endodontist who can properly diagnose the need for a root canal and ensure a successful outcome. The dentist plays a vital role in explaining the treatment plan, addressing patient concerns, and ensuring that all steps are followed to reduce the risk of complications.
8. Root Canal Therapy: Myths and Misconceptions
There are several myths surrounding root canal therapy that often lead to anxiety or fear about the procedure. It is important to address these misconceptions to provide accurate information:
- “Root Canal Therapy is Painful”: With modern anesthesia techniques and pain management strategies, root canal therapy is generally no more painful than a routine filling.
- “A Tooth Treated with Root Canal Will Eventually Need to Be Extracted”: When performed correctly, root canal therapy can
save a tooth for many years or even a lifetime. 3. “Root Canal Therapy Always Fails”: While complications can arise, root canal therapy has a high success rate, especially when performed properly and followed by appropriate restoration.
9. Conclusion
Root canal treatment is a highly effective procedure for preserving damaged teeth and relieving dental pain caused by pulp infections. While the procedure itself can seem daunting, advances in dental technology and techniques have made it safer, quicker, and more comfortable than ever before. By following proper post-treatment care and ensuring timely restoration of the tooth, patients can enjoy a healthy, functional tooth for many years.
Endodontic therapy, when performed appropriately, helps maintain the natural teeth, providing long-term solutions and improving overall dental health. Regular dental checkups and early detection of problems are key to preventing the need for more invasive procedures like extractions.












































Discussion about this post