Tooth pain is a common complaint that affects people of all ages, and one of the most prevalent causes of severe dental discomfort is pulpitis, or inflammation of the dental pulp. The dental pulp is the innermost part of the tooth, consisting of nerves, blood vessels, and connective tissue. When this sensitive area becomes inflamed, it can lead to excruciating pain, sensitivity, and long-term damage if left untreated.
This article provides a detailed, comprehensive guide on pulpitis—its causes, symptoms, diagnosis, and the various treatment methods available. Whether through non-invasive procedures or more intensive treatments like root canal therapy, understanding pulpitis is essential for effective treatment and prevention. By the end of this article, readers will have an in-depth understanding of how to manage pulpitis and the available options for preserving their teeth and alleviating pain.
1. Introduction to Pulpitis
1.1 What is Pulpitis?
Pulpitis refers to the inflammation of the dental pulp, the soft tissue inside a tooth that contains blood vessels, nerves, and connective tissue. The pulp is crucial to the tooth’s overall health, as it supplies nutrients to the tooth and is responsible for its sensory functions. When the pulp becomes irritated or infected, it can cause pain and other symptoms. Pulpitis is often associated with untreated tooth decay, trauma, or other damage to the tooth, which can compromise the pulp’s integrity.
Pulpitis can be categorized into two main types:
- Reversible pulpitis: A mild form of pulp inflammation, where the pulp is still healthy, and the damage is reversible with appropriate treatment. The pain is often intermittent and triggered by external stimuli such as hot or cold temperatures.
- Irreversible pulpitis: A more severe form of pulp inflammation, in which the damage to the pulp is permanent. This type of pulpitis can lead to constant, throbbing pain, and the pulp will eventually need to be removed through a root canal treatment or, in extreme cases, tooth extraction.
1.2 Causes of Pulpitis
The most common causes of pulpitis are untreated tooth decay and tooth trauma. However, several factors can lead to inflammation of the dental pulp, including:
- Tooth decay (cavities): Bacteria can infiltrate the tooth through the enamel and reach the pulp, causing an infection and inflammation.
- Dental trauma: Physical injury to the tooth, such as cracking or chipping, can expose the pulp to infection or irritation.
- Multiple dental procedures: Extensive dental treatments, like large fillings or multiple restorations, can damage the pulp by irritating or exposing it.
- Gum disease: Advanced stages of gum disease can cause inflammation that spreads to the pulp.
- Cracked tooth: Even minor cracks in the enamel can allow bacteria to enter the tooth, leading to pulpitis.
- Bruxism: Grinding or clenching your teeth can exert excessive pressure on the pulp, leading to irritation and inflammation.
- Extreme temperature fluctuations: Exposing teeth to sudden, extreme temperatures, such as eating hot or cold food, can irritate the pulp, especially if the enamel is already weakened.
1.3 Symptoms of Pulpitis
The symptoms of pulpitis vary depending on the severity of the condition and whether the inflammation is reversible or irreversible. Common symptoms include:
1.3.1 Signs of Reversible Pulpitis:
- Sharp or sudden pain: Often triggered by hot or cold temperatures, such as drinking hot beverages or consuming ice cream.
- Pain that subsides after removal of the stimulus: The pain tends to disappear once the irritant is removed or the stimulus is stopped.
- Sensitivity to pressure: Mild pain when chewing or biting.
- No prolonged discomfort: The pain typically does not last long after the trigger is removed.
1.3.2 Signs of Irreversible Pulpitis:
- Severe, constant pain: Persistent throbbing pain that doesn’t go away or is only alleviated temporarily by pain relievers.
- Pain at night: The pain may become worse when lying down or at night, making it difficult to sleep.
- Sensitivity to temperature: Extreme sensitivity to hot or cold that lasts for several seconds or minutes after exposure.
- Swelling and tenderness: Swelling in the gums around the affected tooth and tenderness when touching the area.
- Discoloration: The tooth may appear darker or discolored due to infection or damage to the pulp.
- Foul taste or odor: In cases where the pulp becomes infected, a bad taste or odor may emanate from the tooth.
If left untreated, irreversible pulpitis can progress to an abscess, causing further damage and potential tooth loss.
2. Diagnosis of Pulpitis
2.1 Clinical Examination
The first step in diagnosing pulpitis is a comprehensive clinical examination. The dentist will visually inspect the tooth for signs of decay, fractures, or cracks. They will also evaluate the health of the surrounding gums to detect signs of infection.
2.2 X-rays and Imaging
X-rays are often used to evaluate the extent of the damage and determine if the pulp is affected. An X-ray can reveal the presence of deep cavities, fractures, or infections in the bone surrounding the tooth, which may be indicative of pulpitis.
2.3 Pulp Vitality Tests
To assess the health of the pulp, the dentist may perform vitality tests to gauge the tooth’s response to stimuli. Common tests include:
- Cold test: A cold stimulus, such as ice or cold spray, is applied to the tooth to determine the level of sensitivity. If the tooth reacts excessively to cold or fails to react at all, it may indicate pulpitis.
- Electric pulp test: A mild electric current is passed through the tooth to check for nerve responsiveness. The absence of response may indicate that the pulp is no longer vital (irreversible pulpitis).

3. Treatment Options for Pulpitis
The treatment for pulpitis depends on whether the condition is reversible or irreversible. The goal of treatment is to eliminate the infection or inflammation and preserve the tooth’s function, structure, and appearance.
3.1 Treatment of Reversible Pulpitis
For reversible pulpitis, the inflammation can typically be resolved with conservative treatments. These treatments aim to alleviate symptoms, stop the decay, and protect the pulp from further damage.
3.1.1 Removal of Decay
The first step in treating reversible pulpitis is to remove the decayed portion of the tooth. This is done using dental drills or lasers to clean out the infected tissue and bacteria.
3.1.2 Fillings
Once the decay has been removed, the cavity is cleaned, and a filling is placed to seal the tooth. The filling can be made from materials such as composite resin (tooth-colored) or amalgam (silver). A filling not only restores the tooth’s function but also prevents further bacterial invasion.
3.1.3 Desensitizing Treatments
If the pulpitis is caused by sensitivity, the dentist may apply desensitizing agents to the affected area. These materials can help reduce sensitivity and protect the pulp from further irritation. Fluoride treatments or bonding agents can also be used to strengthen the enamel and reduce the pain triggered by external stimuli.
3.1.4 Temporary Relief and Monitoring
In some cases, the dentist may recommend a temporary filling and observe the tooth over a period of time. This allows the pulp to heal and for the dentist to ensure that the inflammation is resolving.
3.2 Treatment of Irreversible Pulpitis
When pulpitis is irreversible, the damage to the pulp is permanent, and the tooth will not recover on its own. In such cases, more invasive procedures are necessary, such as root canal therapy.
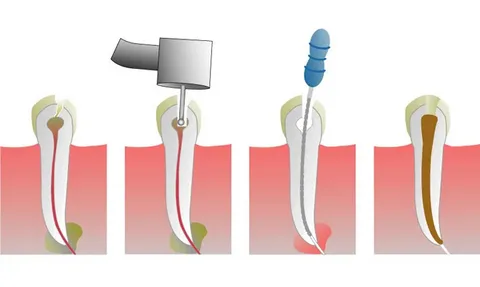
3.2.1 Root Canal Treatment (RCT)
Root canal therapy is the primary treatment for irreversible pulpitis. The procedure involves removing the infected pulp from inside the tooth, cleaning the root canals, and then sealing the tooth. The process is usually performed in several stages:
- Initial cleaning: The dentist will create an access point in the tooth to remove the pulp and clean the canals. Special instruments are used to remove the infected tissue and shape the canals.
- Disinfection: After the pulp is removed, the canals are disinfected to remove bacteria and prevent future infection.
- Sealing: The cleaned canals are filled with a material called gutta-percha to prevent reinfection. The tooth is then sealed with a temporary or permanent filling.
- Post and crown placement: In most cases, the tooth will require a crown to restore its strength and function. A dental crown is placed over the tooth to protect it from future damage.
3.2.2 Post-Root Canal Treatment Care
After root canal therapy, the tooth will be monitored for any signs of infection or complications. Pain and discomfort are common during the initial recovery period, but this should subside within a few days. In some cases, an antibiotic may be prescribed to prevent further infection.
3.3 Tooth Extraction
If the tooth is too damaged or infected for root canal therapy to be effective, tooth extraction may be necessary. This is often a last resort when a tooth cannot be saved due to severe damage or infection. After extraction, the dentist may recommend a replacement option, such as a dental implant, bridge, or dentures to restore the function and aesthetics of the smile.
4. Prevention of Pulpitis
While pulpitis is treatable, preventing it is far better than having to undergo extensive treatment. Several preventive measures can be taken to reduce the risk of developing pulpitis:
4.1 Good Oral Hygiene
Maintaining a rigorous oral hygiene routine is key to preventing tooth decay and gum disease, the leading causes of pulpitis. Brush your teeth at least twice a day with fluoride toothpaste, floss daily to remove plaque and food particles, and use an antiseptic mouthwash to kill harmful bacteria.
4.2 Regular Dental Check-ups
Routine dental check-ups allow the dentist to catch early signs of decay or gum disease before they progress to pulpitis. Regular cleanings remove plaque and tartar buildup, reducing the risk of infection.
4.3 Avoiding Tooth Trauma
Protect your teeth from injury by wearing a mouthguard during sports activities, avoiding chewing on hard objects, and taking care to prevent tooth fractures or chips.
4.4 Treating Sensitivity Early
If you experience frequent tooth sensitivity, seek treatment early to prevent damage to the pulp. Desensitizing toothpaste, fluoride treatments, or other measures can help address the problem before it worsens.
4.5 Diet and Habits
Limit your intake of sugary and acidic foods and drinks, which can erode enamel and increase the risk of cavities. Avoid smoking and excessive alcohol consumption, as these habits can weaken your oral health and contribute to tooth decay and gum disease.
5. Conclusion
Pulpitis is a serious dental condition that can cause significant pain and discomfort if left untreated. Whether caused by cavities, trauma, or other factors, the inflammation of the dental pulp requires prompt attention to prevent further complications. Through early diagnosis, proper treatment, and ongoing preventive care, pulpitis can often be managed effectively, ensuring that teeth remain healthy and functional.
While reversible pulpitis can often be treated with simple procedures such as fillings and desensitizing agents, irreversible pulpitis may require more intensive procedures like root canal therapy or even tooth extraction. By following good oral hygiene practices, scheduling regular dental visits, and taking precautions to avoid tooth damage, individuals can significantly reduce their risk of developing pulpitis and other dental issues.
Taking care of your teeth and seeking professional dental care at the first sign of discomfort can help you avoid the need for more invasive treatments and preserve your natural smile for years to come.












































Discussion about this post