We rarely think about saliva until it’s gone. That persistent, uncomfortable feeling of a dry mouth—sticky, thick, and parched—is more than just an annoyance; it’s a warning sign of a biological system in crisis. Saliva, often taken for granted, is the unsung hero of oral health, a complex biological fluid that performs a symphony of protective functions every minute of every day. When this vital secretion dwindles, a condition known as hyposalivation or xerostomia, the consequences for your teeth and gums can be swift and severe. In this void, saliva substitutes and stimulants have emerged as essential tools, acting as a lifeline for a mouth deprived of its natural defense. But can a bottled solution truly replicate nature’s design? This article delves into the critical role of saliva, the devastating impact of its absence, and how modern science is working to create an artificial stand-in to protect the smiles of millions.
1. More Than Just Water: The Multifaceted, Life-Giving Roles of Saliva
To understand the value of a substitute, one must first appreciate the masterpiece that is natural saliva. It is not merely water; it is a sophisticated serum, a veritable “superfluid” for the mouth.
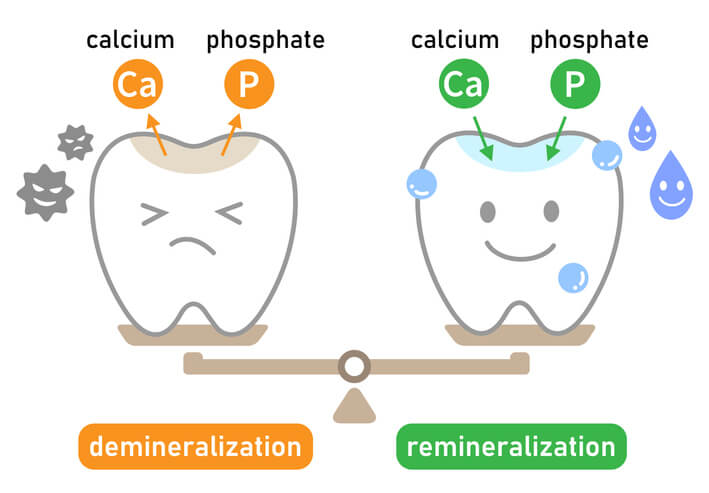
The Ultimate Acid Neutralizer (Buffering): Every time we eat or drink something fermentable, especially carbohydrates and sugars, the bacteria in our plaque produce acid as a byproduct. This acid attack causes the pH in the mouth to plummet, creating an environment where tooth enamel begins to dissolve in a process called demineralization. Saliva is the first responder. It contains bicarbonate ions and proteins that act as powerful buffers, rapidly neutralizing these acids and restoring the mouth to a safe, neutral pH within 20-30 minutes. Without this buffering action, every meal becomes a prolonged acid bath.
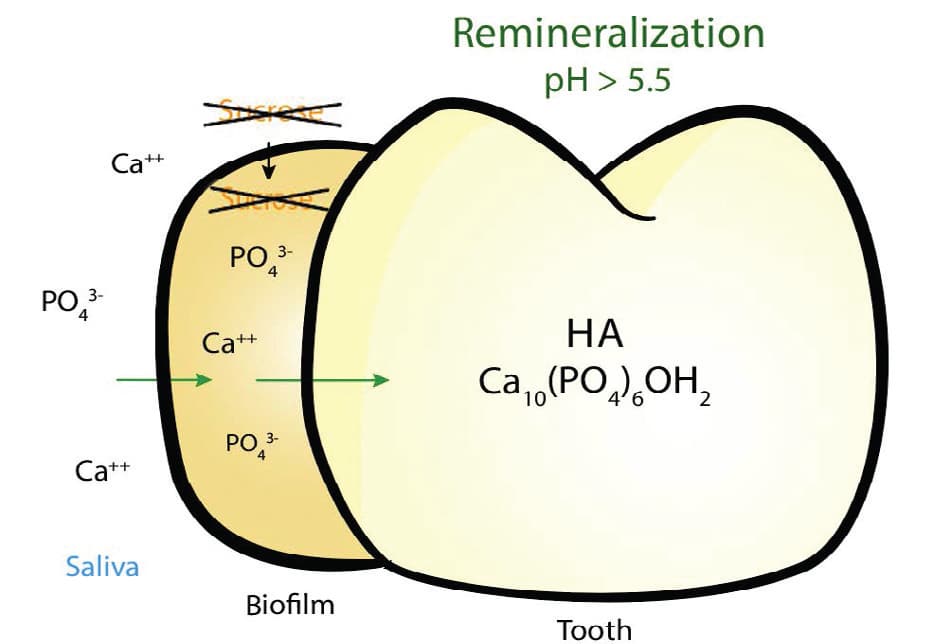
The Natural Tooth Repair Kit (Remineralization): Saliva’s job isn’t just to stop the damage; it’s to reverse it. It is supersaturated with calcium and phosphate ions—the very building blocks of enamel. After an acid attack has softened the enamel, saliva deposits these minerals back into the tooth structure in a healing process called remineralization. Fluoride from toothpaste and water supercharges this process, but saliva provides the essential raw materials.
The Constant Cleanser and Lubricant: Saliva physically washes away food debris and sugars, preventing them from lingering on the teeth and feeding bacteria. Its lubricating properties allow us to speak, taste, and swallow comfortably. It also forms a protective pellicle layer on the teeth, a thin organic film that acts as a barrier against acids and abrasion.
The Antimicrobial Shield: Saliva is packed with immunoglobulins (like IgA), enzymes (like lysozyme and lactoferrin), and other proteins that actively suppress the growth of pathogenic bacteria and fungi, maintaining a balanced oral microbiome.
2. When the Well Runs Dry: The Multitude of Causes Behind Hyposalivation
Dry mouth is not a disease in itself but a symptom of an underlying issue. The causes are numerous and often interconnected.
Medication Side Effects: This is the most common cause of dry mouth. Over 500 medications list xerostomia as a side effect, including:
- Antihistamines (for allergies)
- Decongestants
- Antidepressants and anti-anxiety medications
- Blood pressure medications (diuretics)
- Pain medications
- Muscle relaxants
Systemic Diseases and Conditions: Several medical conditions directly affect salivary gland function.
- Sjögren’s Syndrome: An autoimmune disorder where the immune system attacks the body’s moisture-producing glands, including salivary and tear glands.
- Diabetes: Poorly controlled diabetes can lead to dehydration and reduced saliva flow.
- HIV/AIDS
- Parkinson’s and Alzheimer’s Disease
Medical Treatments:
- Radiation Therapy: Radiation to the head and neck region can irreparably damage salivary gland tissue, often causing a severe and permanent dry mouth.
- Chemotherapy: These drugs can alter the composition and flow of saliva, making it thick and stringy.
Lifestyle Factors: Mouth breathing (often due to nasal congestion), smoking, and high intake of caffeine or alcohol can all contribute to a drier oral environment.
3. The Artificial Lifeline: Understanding Saliva Substitutes and Stimulants
When natural saliva production is compromised, two main categories of products can help: saliva substitutes and saliva stimulants.
Saliva Substitutes (Artificial Saliva): These products are designed to mimic the properties of natural saliva. They are essentially lubricating and moisturizing agents that aim to temporarily wet the oral tissues. Their formulations vary:
- Carboxymethylcellulose (CMC) or Hydroxyethylcellulose-based: These are the most common. They create a lubricating film that coats the mouth, providing relief for one to two hours.
- Mucin-based: Mucin is a key glycoprotein found in natural saliva. Substitutes containing animal-derived mucin are thought to more closely replicate the feel and protective qualities of real saliva.
- Electrolyte-based/Oral Sprays: These often contain calcium and phosphate ions to support remineralization, along with fluoride for added protection.
- Key Feature: Look for products that are pH neutral and contain fluoride. Avoid substitutes with high acidity or sugars like fructose or sorbitol, which can promote decay.
Saliva Stimulants: These products work by encouraging your own salivary glands to produce more fluid.
- Prescription Medications: Drugs like Pilocarpine (Salagen) and Cevimeline (Evoxac) work by stimulating the nervous system that controls salivary glands. They are effective but can have systemic side effects like sweating, flushing, and increased urination.
- Over-the-Counter Options: Sugar-free gum and lozenges are the simplest stimulants. The act of chewing or sucking triggers a reflex salivary flow. Ingredients like xylitol are particularly beneficial as they also help fight cavity-causing bacteria.
4. Maximizing Relief: A Strategic Guide to Using Artificial Saliva Effectively
Using a saliva substitute isn’t like using mouthwash; it requires a consistent, strategic approach to be effective.
Timing is Everything: Don’t wait until your mouth is painfully dry.
- Preemptive Use: Apply the substitute before meals to aid in chewing and swallowing.
- Bedtime is Critical: Saliva flow is naturally lowest at night. Using a longer-lasting gel or ointment formulation right before sleep is crucial to protect your teeth during this vulnerable period.
- Frequent Application: Sprays and rinses have a short duration. Carry a bottle with you and use it frequently throughout the day, as needed.
Proper Application Technique:
- For sprays, aim for the inside of the cheeks and the tongue, not just the roof of the mouth.
- For gels, apply a small amount with a finger or a cotton swab to the gums, palate, and inside of the cheeks.
- Shake the product well before use.
Complementary Strategies:
- Sip Water Constantly: Keep a water bottle with you at all times. This is not a substitute for saliva’s active properties, but it helps with lubrication and rinsing.
- Use a Humidifier: Adding moisture to the air in your bedroom, especially at night, can significantly reduce dry mouth symptoms.
- Avoid Triggers: Limit caffeine, alcohol, and spicy or salty foods, which can exacerbate dryness.
5. Beyond the Bottle: When to Seek Professional Help for the Root Cause
While saliva substitutes are a vital management tool, they are a treatment for the symptom, not the cause. It is imperative to consult your dentist or physician to uncover the underlying reason for your dry mouth.
Red Flags Warranting a Dental/Medical Consultation:
- A persistently dry mouth that doesn’t improve with over-the-counter remedies.
- Difficulty chewing, swallowing, or speaking.
- A change in your sense of taste.
- A burning or sore sensation in your mouth.
- Cracked, split lips or sores at the corners of your mouth (angular cheilitis).
- A dramatic and rapid increase in cavities, especially at the gumline or on the roots of teeth.
What Your Dentist Can Do:
- Diagnose the Pattern of Decay: They can identify the tell-tale signs of “dry mouth caries.”
- Provide High-Fluoride Prescriptions: They can prescribe high-potency fluoride toothpaste (5,000 ppm) or custom fluoride trays to aggressively protect your demineralized teeth.
- Identify and Coordinate Care: Your dentist can help determine if your dry mouth is medication-related and communicate with your physician about possible alternatives or adjustments. They may also run tests to screen for conditions like Sjögren’s Syndrome.
Saliva substitutes are not a perfect replica of nature’s brilliant design, but they are a crucial, life-changing intervention for those suffering from dry mouth. They provide the lubrication and moisture desperately needed for comfort and function, while the best among them offer a degree of biochemical protection. However, they are part of a larger battle plan. By combining the strategic use of these artificial aids with a relentless focus on superior oral hygiene, dietary mindfulness, and a professional investigation into the root cause, you can defend your smile against the silent but devastating threat of a mouth without saliva.












































Discussion about this post