For many, the cover of night brings not restful silence, but a hidden, destructive symphony of grinding and clenching. This involuntary act, known as bruxism, is a common yet often undiagnosed condition that affects a significant portion of the population. Many individuals are entirely unaware they grind their teeth, only learning of it from a sleep partner or a dentist who notices the telltale signs of wear. Bruxism is more than just a noisy nuisance; it is a potent force that can systematically dismantle the structural integrity of your smile, leading to pain, dysfunction, and costly dental repairs. So, what drives this subconscious behavior, and how can it be effectively managed?
Understanding bruxism requires looking at it not as a simple habit, but as a complex physical manifestation with multifaceted origins, primarily rooted in the interplay between sleep physiology and the nervous system. This article will delve into the primary catalysts for bruxism, exploring its strong links to sleep disorders and psychological stress. We will then navigate the spectrum of treatment options, from professionally fabricated dental guards to behavioral therapies, and finally, uncover the sobering long-term effects of leaving this condition untreated.
The Unseen Triggers: Unpacking the Causes of Bruxism
Bruxism is broadly categorized into two types: awake bruxism (occurring during consciousness) and sleep bruxism (occurring during sleep). While their manifestations are similar, their underlying drivers often differ.
1. The Sleep Disorder Connection:
Sleep bruxism is now widely recognized as a sleep-related movement disorder, often coexisting with other sleep disturbances. The most significant link is with Sleep Apnea, particularly Obstructive Sleep Apnea (OSA).
- The Arousal Mechanism: During an apneic event, the airway becomes blocked, leading to a dangerous drop in blood oxygen levels. The brain, in a panic, triggers a micro-arousal—a brief awakening that restores breathing. This arousal is frequently accompanied by a strong jaw clench or grind. The grinding motion is believed to be a reflexive attempt to stimulate the muscles of the upper airway, helping to reopen the passage. In this context, bruxism is not the primary problem but a symptom of a much more serious respiratory issue.
- Other Sleep Factors: Beyond apnea, general sleep disruptions and arousals from any cause (e.g., environmental noises, restless leg syndrome) can trigger bruxism episodes. The brain’s transition between sleep stages is a particularly vulnerable period.
2. The Stress and Anxiety Link:
This is the most commonly cited cause for both awake and sleep bruxism. The modern “fight-or-flight” response, characterized by chronic stress and anxiety, creates a state of heightened neuromuscular tension.
- Awake Bruxism: During the day, individuals may subconsciously clench their jaws as a physical outlet for nervous energy, frustration, or intense concentration. This often occurs during driving, working on a computer, or studying.
- Sleep Bruxism: While the conscious mind sleeps, the subconscious nervous system remains on high alert. The tension accumulated throughout the day is released through nocturnal grinding and clenching. It is the body’s way of metabolizing stress during sleep, albeit in a physically damaging manner.
3. Additional Contributing Factors:
- Medications and Substances: Certain antidepressants (SSRIs), stimulants used for ADHD, and recreational drugs can increase the risk of bruxism.
- Lifestyle: High consumption of caffeine, alcohol, and tobacco has been linked to an increased frequency of grinding.
- Genetics and Anatomy: Bruxism often runs in families, and certain malocclusions (poor bites) may contribute, though this is considered a less significant primary cause than once thought.
The Arsenal of Intervention: Effective Treatment Options
There is no single “cure” for bruxism, as it is often a symptom of a deeper issue. Therefore, effective management is multi-pronged, focusing on protection, addressing root causes, and managing symptoms.
1. The First Line of Defense: Dental Guards (Occlusal Splints)
A custom-fitted dental guard, made from a hard acrylic by a dentist, is the cornerstone of bruxism management. It is crucial to distinguish this from a generic, over-the-counter “boil-and-bite” sports guard.
- How It Works: A professional guard does not stop the grinding behavior. Instead, it acts as a protective barrier, absorbing and distributing the immense forces generated by clenching and grinding. This prevents tooth-on-tooth contact, protecting the enamel from wear and fractures.
- The Professional Advantage: A dentist-designed splint is engineered to create an ideal, stable jaw position, which can help reduce muscle strain on the temporomandibular joints (TMJ) and associated muscles. Over-the-counter guards are often bulky, can disrupt the bite, and may even intensify clenching in an attempt to stabilize the jaw.
2. Addressing the Root Cause:
- Treating Sleep Apnea: If a sleep study confirms OSA, treating it with a CPAP (Continuous Positive Airway Pressure) machine is the most effective intervention. By keeping the airway open, CPAP therapy eliminates the apneic events and the associated micro-arousals, which often dramatically reduces or resolves sleep bruxism.
- Stress Management and Behavioral Therapy: For stress-related bruxism, cognitive-behavioral therapy, mindfulness, meditation, and regular exercise can be profoundly effective in lowering the body’s overall stress load. For awake bruxism, biofeedback—learning to recognize jaw clenching and consciously relax the muscles—can help break the habit.
3. Symptomatic and Adjunct Therapies:
- Physical Therapy: Targeted exercises can stretch and relax the jaw, neck, and shoulder muscles, alleviating pain and improving range of motion.
- Medications: In severe, short-term cases, muscle relaxants or Botox (botulinum toxin) injections may be considered. Botox works by partially paralyzing the masseter muscles, reducing their grinding force, but it does not address the underlying trigger.
The High Cost of Inaction: Understanding the Long-Term Effects
Choosing to ignore bruxism is a decision with significant and often irreversible consequences for oral and overall health.
- Catastrophic Tooth Damage:
- Abrasion and Attrition: The constant grinding wears down the chewing surfaces of the teeth, making them shorter and flatter. In advanced cases, it can wear through the enamel, exposing the sensitive dentin and leading to severe sensitivity and an increased risk of decay.
- Fractures: The immense pressure can cause teeth to crack, chip, or fracture, necessitating crowns, root canals, or even extractions.
- Failed Dental Work: Crowns, fillings, and veneers are highly susceptible to damage from grinding forces, leading to premature failure and costly replacements.
- Temporomandibular Joint Disorders (TMD):
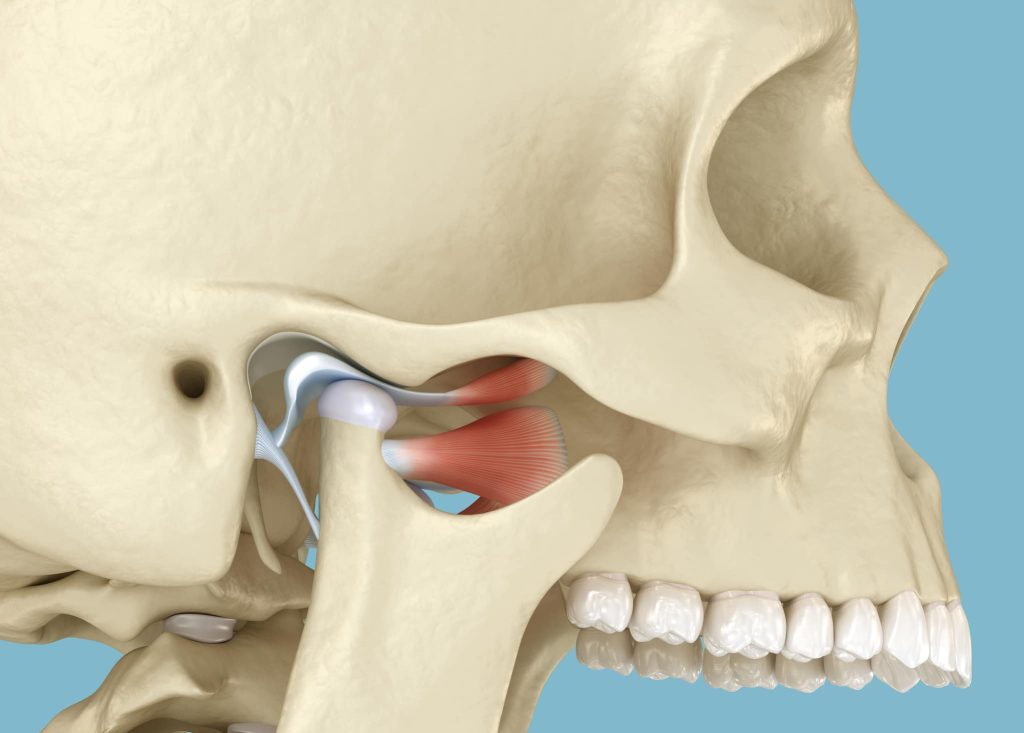
The TMJs are the complex hinges connecting your jaw to your skull. The chronic, excessive force of bruxism places tremendous strain on these joints and the surrounding muscles, leading to:- Jaw pain, clicking, and popping
- Locking of the jaw
- Headaches and earaches
- Pain that radiates to the neck and shoulders
- Chronic Musculoskeletal Pain:
The masseter and temporalis muscles, which power the jaw, can become hypertrophied (enlarged) and chronically fatigued, leading to persistent facial pain and tension-type headaches, often misdiagnosed as migraines. - Sleep Disruption and Daytime Fatigue:
Even if the individual is not consciously awakened by their grinding, the micro-arousals associated with bruxism disrupt the natural sleep cycle. This leads to non-restorative sleep, resulting in daytime fatigue, irritability, and poor concentration.
Conclusion: From Destructive Habit to Managed Condition
Bruxism is a potent reminder of the deep connection between mind, body, and oral health. It is not a behavior to be taken lightly. Successfully managing it requires a diagnostic approach to identify its root cause—be it a sleep disorder like apnea or the physical manifestation of chronic stress.
The treatment path is a partnership between patient and provider. It begins with the essential protection of a custom dental guard to prevent physical damage, but it must extend to addressing the underlying trigger, whether through CPAP therapy, stress reduction, or lifestyle changes. By taking proactive steps, you can silence the grind, protect your smile from irreversible damage, and reclaim restful, pain-free days and nights.













































Discussion about this post