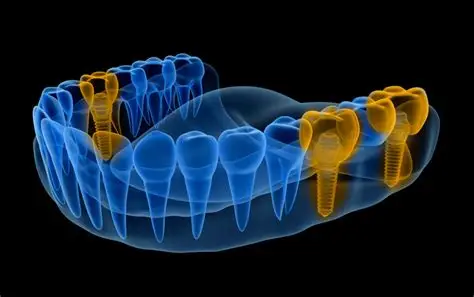
The success of dental implants represents one of the most significant achievements in modern dentistry, offering a predictable and life-changing solution for tooth loss. For decades, the core principles have remained largely unchanged: a biocompatible titanium screw is surgically placed into the jawbone, where it integrates through a process called osseointegration, and is then restored with a crown. While this protocol is highly successful, the future promises a revolution that will make implants smarter, their integration faster and more reliable, and their placement profoundly less invasive. We are moving from a era of mechanical replacement to an age of biological integration and digital intelligence.
The next generation of implant dentistry is being shaped by breakthroughs in materials science, biotechnology, and digital surgery. This evolution aims not only to improve success rates but to redefine the entire patient experience, from reducing healing times to creating implants that actively monitor health. This article will explore three key frontiers of innovation: the development of “smart” implants with biosensing capabilities, groundbreaking approaches to accelerate and enhance osseointegration, and the rise of minimally invasive, flapless surgical techniques guided by advanced digital planning.
The Sentient Screw: The Era of Smart Implants
The passive titanium fixture is evolving into an active, data-generating medical device. Smart implants are being developed with integrated microsensors and nanotechnology to provide real-time, objective health monitoring.
1. Biosensing and Diagnostic Capabilities:
These futuristic implants could be coated with or constructed from materials that react to specific biological markers. They would be capable of:
- Monitoring Osseointegration: Sensors could detect micromotion at the bone-implant interface, providing an early warning of failed integration or peri-implantitis long before it becomes visible on a radiograph. This would allow for proactive intervention.
- Detecting Infection (Peri-Implantitis): Nanosensors functionalized to react with specific inflammatory cytokines or bacterial byproducts (e.g., from P. gingivalis) could change color or emit a signal when infection thresholds are reached. A dentist could use a specialized device to “read” the implant’s status during a check-up.
- Tracking Load and Occlusal Forces: Embedded micro-strain gauges could measure the chewing forces exerted on the implant. This data could be transmitted to a smartphone app, alerting the patient and dentist to parafunctional habits like bruxism that could jeopardize the long-term health of the implant, the bone, and the restoration.
2. Drug-Eluting and Therapeutic Implants:
Moving beyond diagnostics, the implant itself could become a delivery system for therapeutic agents. The surface or an internal reservoir could be coated with a biodegradable polymer containing:
- Osteoinductive Growth Factors: (e.g., BMP-2) to actively stimulate bone formation.
- Local Antibiotics or Antimicrobial Peptides: To prevent infection in the critical early healing phase, especially valuable for high-risk patients.
Forging a Stronger Bond: Accelerating and Improving Osseointegration
The 3-6 month healing period for osseointegration is a major factor in the overall treatment timeline. Future innovations are focused on making this process faster, more predictable, and possible even in compromised bone.
1. Advanced Surface Bio-engineering:
While current implants use roughened surfaces, the future lies in nano-topography. By creating surfaces with specific patterns at the nanometer scale (pits, tubes, pillars), researchers can directly influence cell behavior. These nano-engineered surfaces can:
- Enhance the adsorption of proteins that promote bone cell attachment.
- Directly stimulate mesenchymal stem cells to differentiate into osteoblasts (bone-forming cells) more rapidly.
- Create a super-hydrophilic (water-attracting) surface that immediately wicks blood and proteins, significantly accelerating the initial healing response.
2. Biomimetic and Bioactive Coatings:
The next step is moving from a surface that bone cells like to a surface that actively commands them to grow.
- Bioactive Glass Coatings: Materials like 45S5 Bioglass® react with physiological fluids to form a hydroxycarbonate apatite layer that is chemically similar to bone mineral, creating an intimate and strong bond.
- Peptide-Based Coatings: Short, synthetic amino acid sequences (peptides) like RGD can be grafted onto the implant surface. These peptides are recognized by cell membrane receptors, acting as “landing pads” that dramatically increase the speed and strength of bone cell attachment.
3. The Use of Electromagnetic and Laser Therapy:
Post-operatively, technologies like Pulsed Electromagnetic Field (PEMF) therapy or Low-Level Laser Therapy (LLLT) could become standard. These non-invasive treatments have been shown to upregulate cellular activity and increase blood flow, potentially cutting osseointegration times by a significant margin.
The Precision Puncture: The Shift to Minimally Invasive Procedures
The traditional implant surgery involving flap elevation, sutures, and significant post-operative discomfort is being replaced by protocols that are more precise and far gentler.
1. Fully Guided Flapless Surgery:
This represents the pinnacle of digital dentistry. Using CBCT scans and intraoral digital impressions, a virtual surgery is planned in 3D software with sub-millimeter accuracy. From this plan, a surgical guide is 3D-printed. This guide fits perfectly over the patient’s teeth or gums and has metal sleeves that dictate the exact position, angle, and depth of the osteotomy (bone preparation). The surgeon uses the guide to place the implant through a tiny punch-hole in the gum, without the need for any incisions or sutures.
Benefits of this approach include:
- Dramatically Reduced Trauma: No flap means minimal bleeding, swelling, and post-operative pain.
- Unparalleled Precision: The implant is placed exactly as planned, ensuring optimal positioning for the final restoration and avoiding critical anatomical structures.
- Faster Healing and Immediate Function: The preserved blood supply and lack of sutures allow for very rapid soft-tissue healing. In many cases, this facilitates immediate loading (placing a temporary tooth on the implant the same day).
2. Robotics and Dynamic Navigation:
Beyond static guides, the future lies in dynamic systems. Robotic arms, controlled by the digital plan, can hold and position the drill with superhuman steadiness and accuracy. Alternatively, dynamic navigation systems use infrared cameras to track the position of the patient’s jaw and the surgical handpieces in real-time, projecting the planned implant position and the actual drill position onto a screen. This is like having a GPS for implant surgery, allowing for adjustments on the fly while still maintaining a flapless, minimally invasive approach.
Conclusion: A Biologically Integrated, Digitally Perfect Future
The future of implant dentistry is not merely incremental improvement; it is a fundamental reimagining of the therapy. The passive screw will give way to a smart, therapeutic device that monitors health and promotes healing. The long, uncertain wait for osseointegration will be shortened through bio-engineered surfaces that actively command bone growth. And the invasive surgery of the past will be rendered obsolete by digital and robotic systems that place implants with pinpoint accuracy through a virtually painless, flapless procedure.
These converging innovations—smart implants, enhanced osseointegration, and minimally invasive surgery—promise a future where tooth replacement is not just a mechanical substitution, but a seamless, biologically integrated, and patient-centric process that is faster, safer, and more predictable than ever before.













































Discussion about this post